Assessments
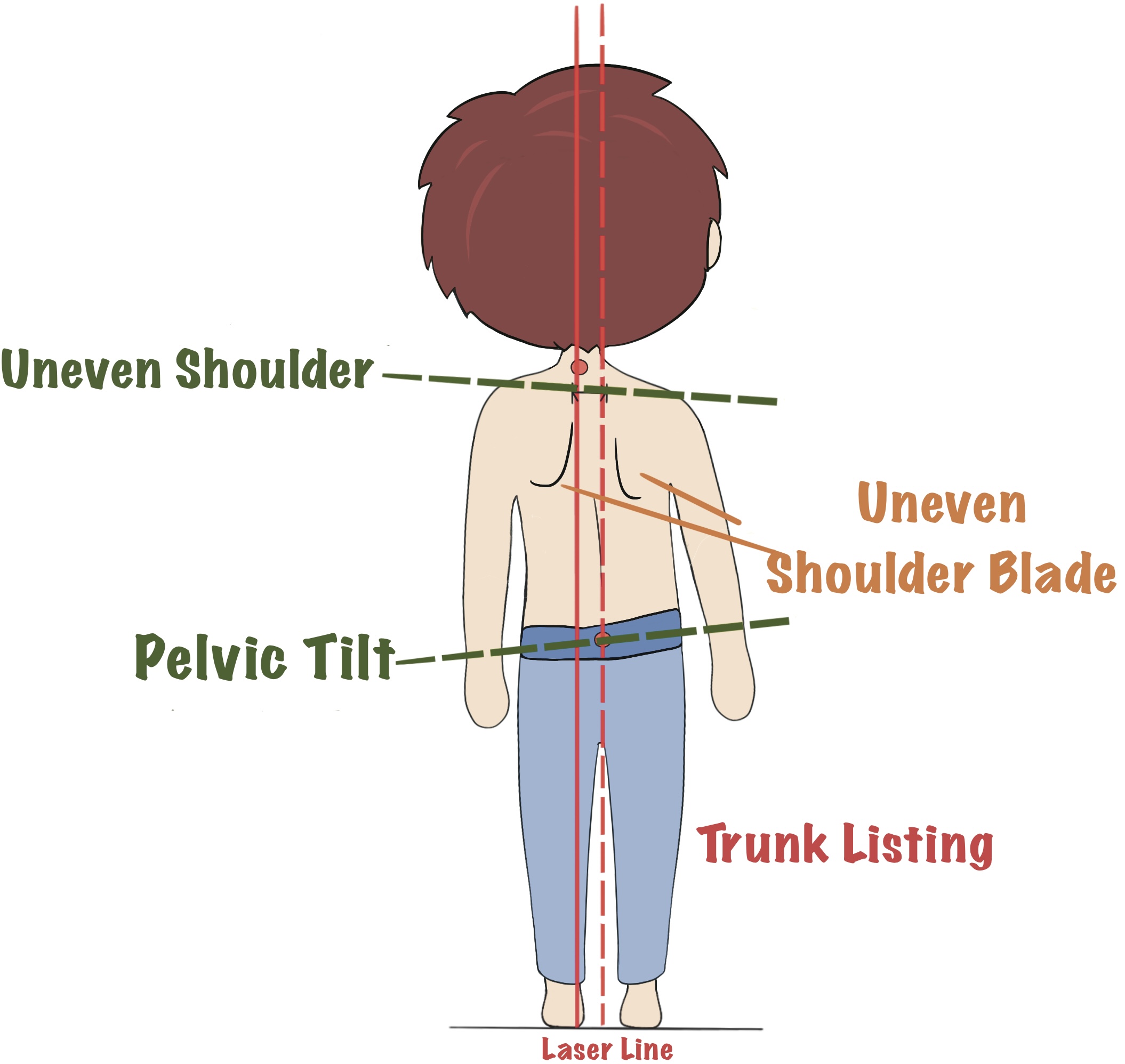
Physical Observation
Scoliosis can be observed by body asymmetry such as uneven shoulders, shoulder blade, thoracic hump, loin depression or pelvic tilt. In severe cases, appearance and cardiopulmonary function could also be affected [1,2]. Observation of the body shape and contour is a simple method to assess the potential of having scoliosis, which may indicate the need for further investigations while it would be difficult for mild scoliosis as those subtle changes may not be noticeable.
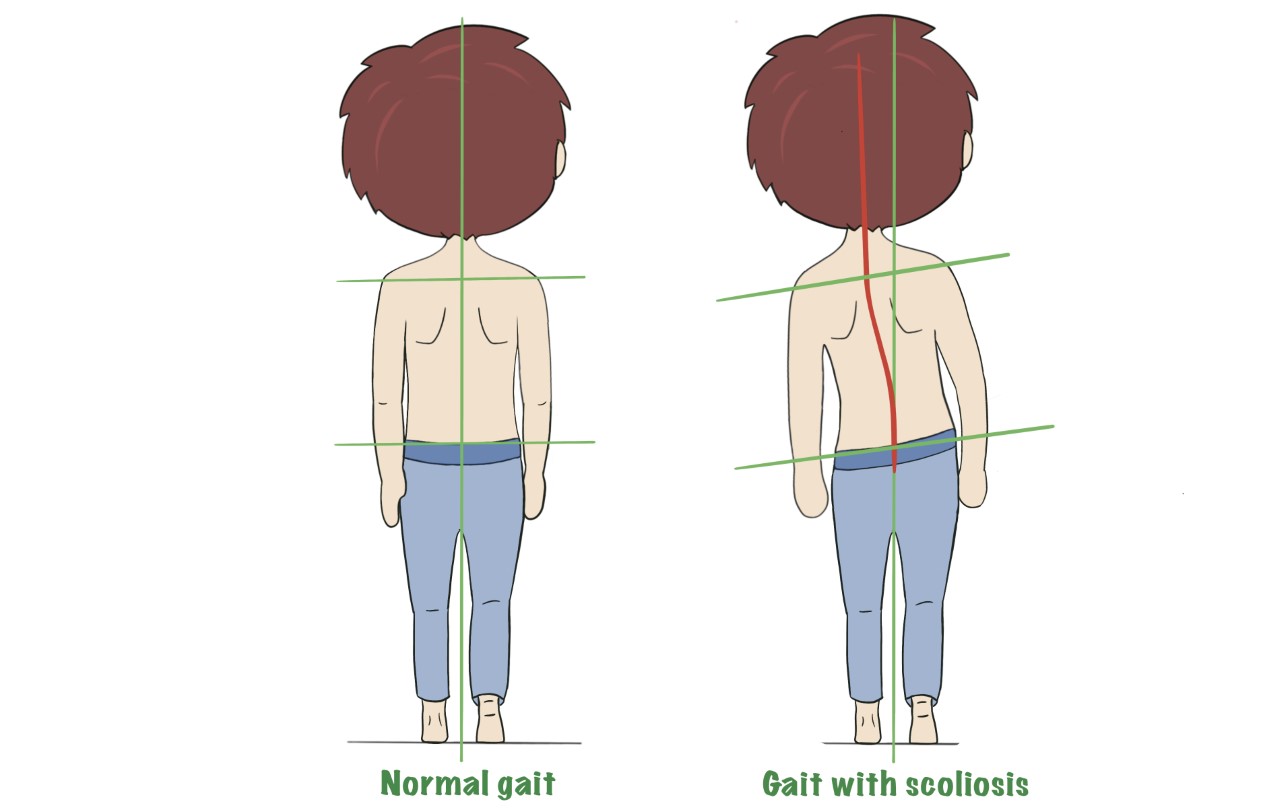
Adam's Forward Bend Test
The Adam’s forward bending test is a useful tool to detect structural or postural scoliosis. This method is commonly used in scoliosis screening programs at schools [3-5].
During the assessment, the child is required to bend his or her trunk forward to a horizontal level with feet slightly apart, knees extended with palms together and placed in-between the knees. Clinician will measure the angle of trunk inclination by moving an inclinometer named Scoliometer along the child’s back over the spinous processes. The measured tilting angle greater than 5 degrees may indicate a potential scoliosis. With the forward bending trunk, clinician can also observe body asymmetry of uneven shoulder blade, rib hump or loin depression resulting from vertebral rotation [6].

Adam's Forward Bend Test
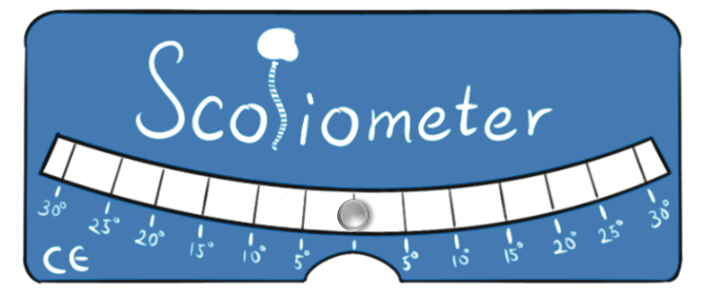
Scoliometer
Back Profile
The SpineScan3D is a recent development in Hong Kong, which allows the back-profile’s screening to be performed at schools. This portable device that can be connected with a smartphone, which allows to detect and record the trunk rotation in forward bending (same to the “Adam’s forward bending test”) or upright position.
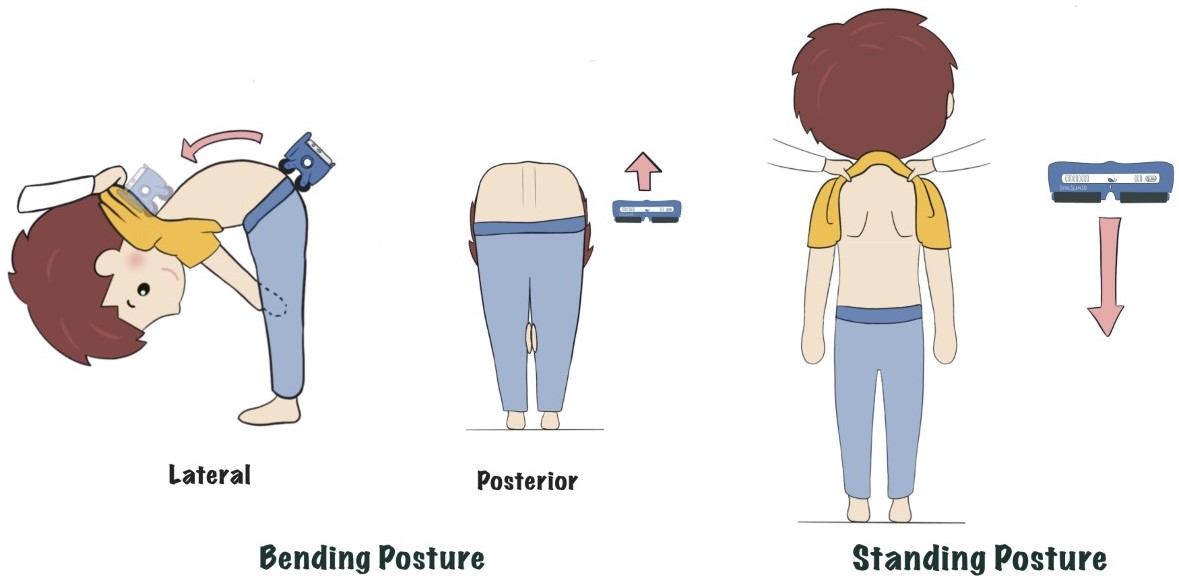
SpineScan3D
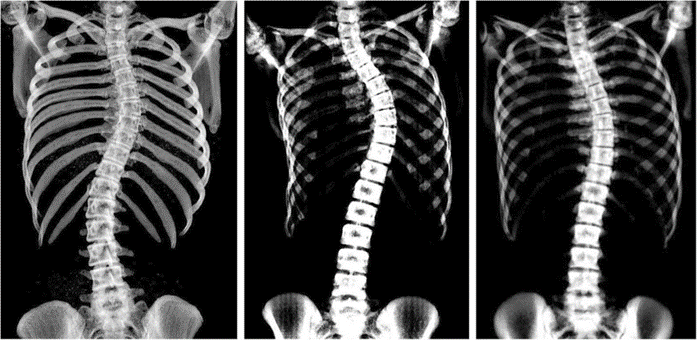
X-Ray & Cobb Angle
X-Ray imaging is often used to assess scoliosis severity in which the Cobb method is endorsed by the Scoliosis Research Society as a “gold standard” for scoliosis evaluation [7,8]. The measured Cobb Angle is a standard measurement to diagnose and track the progression of scoliosis. A Cobb angle larger than 10o can be regarded as having Scoliosis (view more…) [9].
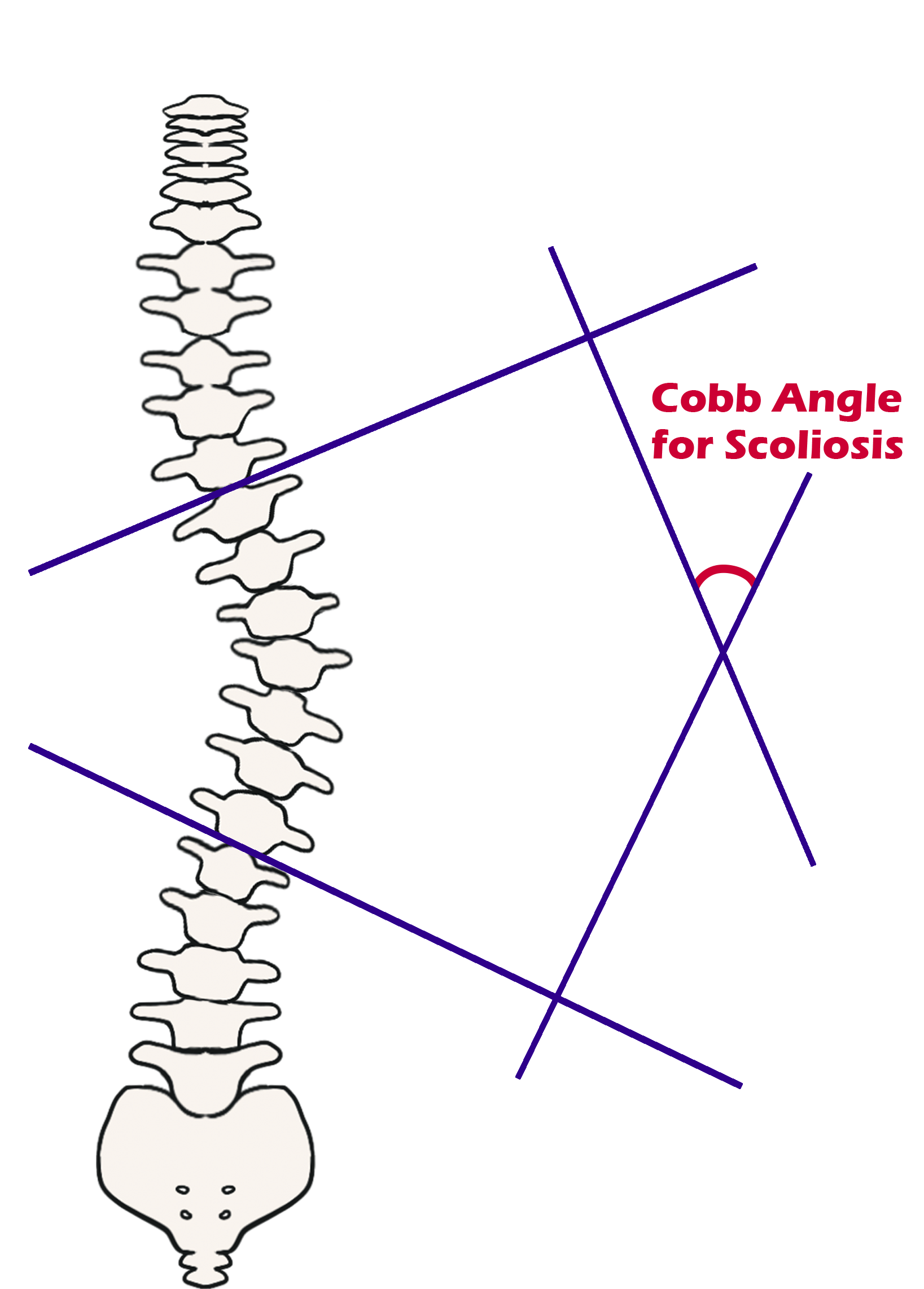
Cobb angle
Ultrasound Scanning
Ultrasound is radiation-free and more cost effective compared to X-ray imaging. Therefore, it is suitable to be used in assessing progress of scoliosis in children across the high risk period [10,11]. Two ultrasound imaging systems including a stationary system "Scolioscan Station" and portable system “Scolioscan Air” have been developed recently by The Hong Kong Polytechnic University. The two systems are used in the “Jockey Club Children’s Spine Care Community Project” to estimate the severity of scoliosis of children.
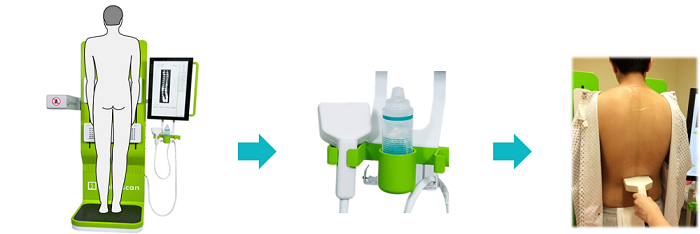
Procedure of using Scolioscan Station
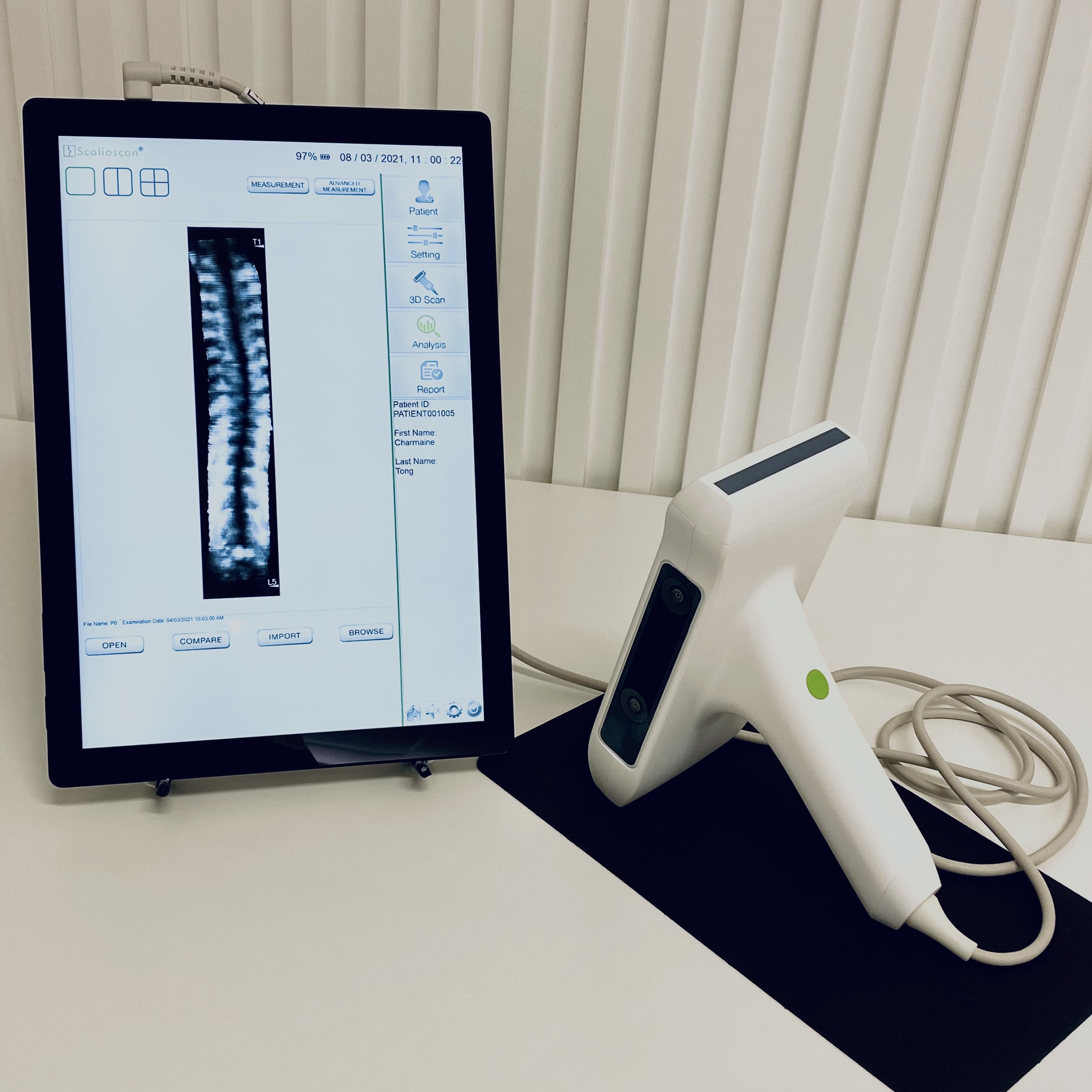
Scolioscan Air
Magnetic Resonance Imaging (MRI)
MRI combines computer technology, radio waves and a magnetic field to generate images of body tissues in different anatomical planes. MRI is non-invasive and radiation-free imaging technique which makes it an attractive assessment method for scoliosis [12-14]. It can produce detailed images of the soft tissues including intervertebral discs, spinal cord and nerves. Contraindications for MRI include pacemakers, cerebral aneurysm clips and metallic implants. However, it is costly and expert dependent [15].

MRI image of scoliosis
Computed Tomography (CT)
CT uses computer technology in combining X-ray measurements taken from different angles to produce cross-sectional images of the body. CT can produce detailed images of the bone, spinal cord and intervertebral discs that facilitate diagnosis of spinal deformities. CT is useful in patients who are not suitable to have MRI such as those with metal implants or pacemakers [16,17].
CT image of scoliosis
EOS system
The EOS X-ray imaging system is able to produce full body stereo-radiographic images in either standing or seated positions with ultra-low dose of radiation [18]. Using the built-in software (SterEOS), 3D images of the skeleton system can be reconstructed. Therefore, it is very useful for diagnosing spinal deformities such as scoliosis, which is considered as a 3D deformity [19].

EOS system
Reference
-
S. H. Service. "Scoliosis." www.studenthealth.gov.hk/english/health/health_bsh/health_bsh_sco.html.
-
A. J. Danielsson, R. Hasserius, A. Ohlin, and A. L. Nachemson, "Health-related quality of life in untreated versus brace-treated patients with adolescent idiopathic scoliosis: a long-term follow-up," Spine, vol. 35, no. 2, pp. 199-205, 2010.
-
A. Clarke, A. Jones, M. O'Malley, and R. McLaren, ABC of spinal disorders. John Wiley & Sons, 2009.
-
J. P. Horne, R. Flannery, and S. Usman, "Adolescent idiopathic scoliosis: diagnosis and management," American family physician, vol. 89, no. 3, pp. 193-198, 2014.
-
B. V. Reamy and J. Slakey, "Adolescent idiopathic scoliosis: review and current concepts," American family physician, vol. 64, no. 1, p. 111, 2001.
-
W. P. Bunnell, "An objective criterion for scoliosis screening," The Journal of bone and joint surgery. American volume, vol. 66, no. 9, pp. 1381-1387, 1984.
-
T. Vrtovec, F. Pernuš, and B. Likar, "A review of methods for quantitative evaluation of spinal curvature," European spine journal, vol. 18, no. 5, pp. 593-607, 2009.
-
A. Oestreich, L. W. Young, and T. Y. Poussaint, "Scoliosis circa 2000: radiologic imaging perspective," Skeletal radiology, vol. 27, no. 11, pp. 591-605, 1998.
-
J. Cobb, "Outline for the study of scoliosis," Instr Course Lect AAOS, vol. 5, pp. 261-275, 1948.
-
Y. P. Zheng, T. T. Y. Lee, K. K. L. Lai, B. H. K. Yip, G. Q. Zhou, W. W. Jiang, J. C. W. Cheung, M. S. Wong, B. K. W. Ng, and J. C. Y. Cheng, "A reliability and validity study for Scolioscan: a radiation-free scoliosis assessment system using 3D ultrasound imaging," Scoliosis and spinal disorders, vol. 11, no. 1, p. 13, 2016.
-
C. W. J. Cheung, S. Y. Law, and Y. P. Zheng, "Development of 3-D ultrasound system for assessment of adolescent idiopathic scoliosis (AIS): and system validation," in 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 2013: IEEE, pp. 6474-6477.
-
R. M. Schwend, W. Hennrikus, J. E. Hall, and J. B. Emans, "Childhood scoliosis: clinical indications for magnetic resonance imaging," The Journal of bone and joint surgery. American volume, vol. 77, no. 1, pp. 46-53, 1995.
-
R. J. Davids, W. E. Chamberlin, and W. D. Blackhurst, "Indications for Magnetic Resonance Imaging in Presumed Adolescent Idiopathic Scoliosis," The Journal of Bone & Joint Surgery, vol. 86, no. 10, pp. 2187-2195, 2004, doi: 10.2106/00004623-200410000-00009.
-
D. K. Lewonowski, D. J. King, and D. M. Nelson, "Routine Use of Magnetic Resonance Imaging in Idiopathic Scoliosis Patients Less than Eleven Years of Age," Spine, vol. 17, no. 6 Suppl, pp. S109-S116, 1992.
-
A. M. Ferreira, F. Costa, A. Tralhão, H. Marques, N. Cardim, and P. Adragão, "MRI-conditional pacemakers: current perspectives," Medical Devices (Auckland, NZ), vol. 7, p. 115, 2014.
-
V. Cassar-Pullicino and S. Eisenstein, "Imaging in scoliosis: what, why and how?," Clinical radiology, vol. 57, no. 7, pp. 543-562, 2002.
-
H. Kim, H. S. Kim, E. S. Moon, C.-S. Yoon, T.-S. Chung, H.-T. Song, J.-S. Suh, Y. H. Lee, and S. Kim, "Scoliosis imaging: what radiologists should know," Radiographics : a review publication of the Radiological Society of North America, Inc, vol. 30, no. 7, pp. 1823-1842, 2010, doi: 10.1148/rg.307105061.
-
T. Illés and S. Somoskeöy, "The EOS™ imaging system and its uses in daily orthopaedic practice," International orthopaedics, vol. 36, no. 7, pp. 1325-1331, 2012.
-
S. Kato, C. Debaud, and R. D. Zeller, "Three-dimensional EOS analysis of apical vertebral rotation in adolescent idiopathic scoliosis," Journal of Pediatric Orthopaedics, vol. 37, no. 8, pp. e543-e547, 2017.