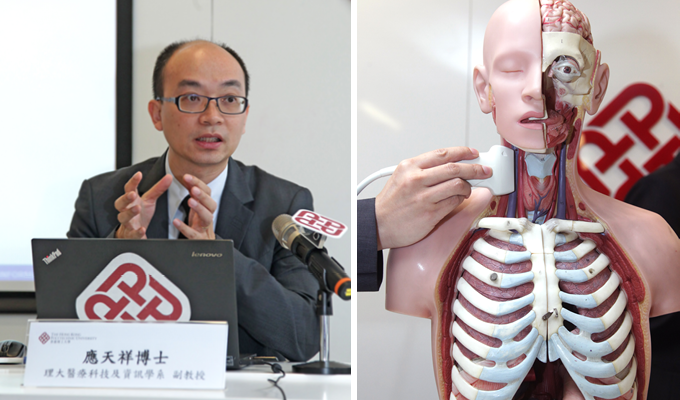
Some people doubt that nasopharyngeal carcinoma patients who received radiotherapy have higher risk of stroke. In this issue, Dr Michael Ying at the Department of Health Technology and Informatics shared the findings of a recent study that would offer an answer to this question.
What are the influences of radiotherapy on nasopharyngeal carcinoma (NPC) patients?
There is a high prevalence of cervical lymph node metastasis in NPC patients. Therefore, neck radiotherapy is commonly used in the treatment process. However, ionising radiation in that therapy will damage the carotid artery and can lead to the development of carotid atherosclerosis, which may result in cerebrovascular events such as transient ischemic attack and stroke.
Please briefly introduce your recent related study.
With this possibility in mind, Prof. Yip Shea-ping, Dr Vincent Wu and I conducted a study to evaluate and compare the degree of carotid atherosclerosis in 69 NPC patients treated with radiotherapy, 70 patients with type 2 diabetes mellitus (DM) and 76 healthy controls without both conventional cardiovascular risk factors and previous radiotherapy. Parameters (including carotid intima-media thickness, carotid arterial stiffness, presence of carotid plaque and carotid stenosis) were assessed using ultrasonography (a safe, non-invasive and cost-effective imaging modality).
What were the findings?
The results indicated that radiation-induced carotid atherosclerosis occurred in 87% of the post-radiotherapy NPC patients. The situation was more severe than that in DM patients and healthy controls in terms of a stiffer carotid artery wall and a higher carotid plaque burden. With a higher prevalence and severity of carotid atherosclerosis, the risk of having a stroke in post-radiotherapy NPC patients is thus higher compared to non-irradiated controls.
What were the recommendations in the follow-up treatment of patients?
The study has enhanced our understanding of the potential variations between radiation-induced and spontaneous carotid atherosclerosis, which might offer a justification for assessing carotid atherosclerosis in routine follow-ups for NPC patients. We recommended oncologists to well control and adjust the dose of radiotherapy for patients so as to avoid unnecessary damage to the normal cells in the neck and surrounding areas; and to perform ultrasound carotid evaluation for NPC patients at least biennially in the four years after radiotherapy.