Bunion is a common foot problem. It not only affects foot’s appearance, but also causes pains and walking problems. In fact, the problems can be prevented from worsening without breaking the patients’ bones in the treatment. In this issue, Dr Aaron Leung Kam-lun at PolyU’s Interdisciplinary Division of Biomedical Engineering shared the findings of a joint study on the effectiveness of “Syndesmosis” — a non-bone-breaking approach to improve the foot functions of patients with bunions.
What is a bunion/hallux valgus? What causes bunions?
Bunion is a protrusion on the side of the big toe. Medically called “hallux valgus deformity complex”, it is one of the forefoot problems. Hallux valgus means the outward tilting of the big toe. The associated forefoot problems include widening of the forefoot, clawed toes, collapsed arches, calluses and even a bunionette on the little toe. Profound hallux valgus leads to patients’ imbalance, joint dysfunction and pains on foot, calf and back.
In general, bunion is a deformity formed by displaced normal bones due to failure of their supporting ligaments on the big toe and the first metatarsal bone. In Hong Kong, approximately one-third of female adults have bunion with the male-female proportion of 1:9. Female patients suffered from the ligament laxity are mainly affected by female hormone, 80% presented by heredity; and habitual wearing of high-heels or pointed shoes worsens the hallux valgus deformation due to compression.
What are the remedial treatments commonly used? How can "Syndesmosis" help without breaking a patient’s bone?
There are non-surgical approaches (such as foot orthoses, night-time bunion splints) and surgeries for remedying bunions. Currently, 90% of surgeries adopt the bone-breaking approach, aiming at improving foot functions and relieving pains. There are, however, risks of displacement and causing other complications.
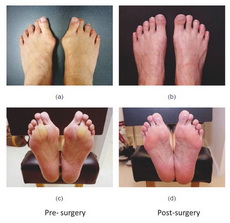
A non-bone breaking approach called “Syndesmosis” was introduced to Hong Kong by orthopedicist Dr Daniel Wu Yiang. Without breaking a patient’s bones, this approach can re-align and re-stabilize the displaced but normal bones of the bunion foot by tying the displaced and loose first metatarsal bone to the adjacent second metatarsal bone. It triggers the body to create a syndesmosis fibrous bridge automatically to connect and stabilize it to the second metatarsal bone. This non-bone breaking surgery results in 90% of success rate with fast recovery. Compared with bone-breaking surgeries, this approach is considered a treatment method without associated pains, metatarsal fractures or secondary problems.
Please briefly introduce the background of your recent study. What are the findings?
In collaboration with the Center for Non-Bone Breaking Bunion Surgery, our study retrospectively assessed 27 patients’ foot functions after taking the bilateral Syndesmosis procedure from mid-2008 to early-2009. In the study, participants walked in flat shoes with insole sensors; the plantar pressure was measured and analyzed while walking.
The study has shown that in two years after the surgery, patients’ mean maximum force under the hallux region increased significantly from 20.6% to 35.2% of the body weight and that of the second and third metatarsal bones decreased from 43.9% to 34.2%. These data reflected that the restoration of functions of patients’ hallux with pains relieved, thereby enabling them to walk with force on pre-existing areas.
In summary, this study has confirmed the effectiveness of non-bone breaking Syndesmosis in restoring the foot functions of patients with bunions.